SAN DIEGO, Aug. 3, 2022 /PRNewswire/ — New research reported at the Alzheimer’s Association International Conference® (AAIC®) 2022 covered the breadth of Alzheimer’s and dementia research, including the basic biology of aging and the brain, risk factors and prevention strategies, and caregiving and living well with the disease.
AAIC is the premier annual forum for presentation and discussion of the latest Alzheimer’s and dementia research. This year’s hybrid conference event took place both virtually and in-person in San Diego and attracted over 9,500 attendees and more than 4,000 scientific presentations.
“With record public and private research investment it’s an exciting time for Alzheimer’s and dementia research,” said Heather M. Snyder, Ph.D., Alzheimer’s Association vice president of medical and scientific relations. “Researchers are advancing our understanding of the disease by exploring biomarkers, discovering potential ways to reduce risk, and working to move promising treatments and diagnostic tools forward into clinical testing. The Alzheimer’s Association is leading the fight through funding, convening, publishing, partnerships, advocacy and services.”
Advances in Treatments, Clinical Trial Results
The Alzheimer’s Association highlighted results from a variety of clinical trials at AAIC 2022. Encouraging and supporting a diverse treatment pipeline is essential to achieving the Association’s vision of a world without Alzheimer’s and all other dementia. Here are two examples:
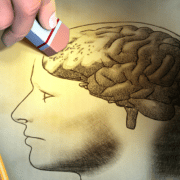
The EXERT Study is the longest-ever Phase 3 study of exercise in older adults with mild cognitive impairment (MCI). The results, first reported at AAIC 2022, are especially noteworthy since the trial was conducted during the COVID-19 pandemic — 80% of participants complied with their exercise regimen and completed the study. After 12 months, people with MCI in both the aerobic exercise intervention arm and stretching arm showed no cognitive decline. A comparison group of other older adults with MCI showed significant cognitive decline over 12 months. The findings from EXERT suggest that regular physical activity, even modest or low exertion activity such as stretching, may protect brain cells against damage.
At AAIC 2022, T3D Therapeutics reported positive interim results from their Phase 2 trial of T3D-959, which seeks to overcome insulin resistance in the brain and restore the brain’s metabolic health. These encouraging preliminary results are a positive sign, and final results are anticipated in 2023. As understanding of the biological underpinnings of Alzheimer’s expands, the opportunity to advance novel approaches such as T3D-959 will also expand.
Also at AAIC, the Alzheimer’s Association announced the launch of the Alzheimer’s Network for Treatment and Diagnostics (ALZ-NET), which will collect long-term clinical and safety data from patients treated with FDA-approved Alzheimer’s disease therapies in real world clinical settings. ALZ-NET is the first network developed specifically for new FDA-approved Alzheimer’s treatments, collecting evidence on effectiveness and side effects over a long period of time.
Experiences of Racism Associated with Poor Memory, Increased Cognitive Decline
Experiences of structural, interpersonal and institutional racism are associated with lower memory scores and worse cognition in midlife and old age, especially among Black individuals.
- In a study of nearly 1,000 middle-aged community-dwelling adults (55% Latinx; 23% Black; 19% White), exposure to interpersonal and institutional racism was associated with lower memory scores; the associations were strongest in Black individuals. Experiences of structural racism were associated with lower episodic memory among all racial and ethnic groups included in the study.
- In a study of 445 Asian, Black, Latino, White and multiracial people age 90 and above, individuals who experienced wide-ranging discrimination throughout life had poorer long-term memory in late life compared to those who experienced little to no discrimination.
History of Hypertensive Disorders During Pregnancy Linked to Increased Risk of Dementia
Hypertensive disorders of pregnancy (HDP) — conditions of high blood pressure including chronic/gestational hypertension and preeclampsia — have been strongly linked to heart disease in later life, but before today, little research has connected these disorders with cognition. Experiences of high blood pressure disorders during pregnancy are associated with an increased risk of vascular dementia and accelerated brain aging, according to several studies at AAIC 2022:
- Women with a history of HDP were more likely to develop vascular dementia — a decline in thinking skills caused by conditions that block or reduce blood flow to the brain — later in life, compared to women with non-hypertensive pregnancies.
- Experience of HDP, specifically high blood pressure during pregnancy, was associated with white matter pathology, a predictor of accelerated cognitive decline, 15 years after pregnancy.
- Women with severe preeclampsia had significantly higher levels of beta amyloid, an Alzheimer’s-related brain change, as measured in blood compared to those with non-hypertensive pregnancies.
Persistent Loss of Smell Due to COVID-19 Closely Connected to Long-Lasting Cognitive Problems, and ICU Stays May Double Risk of Dementia in Older Adults
New insights into factors that may predict, increase or protect against the impact of COVID-19 and the pandemic on memory and thinking skills were revealed by multiple studies at AAIC 2022. A research group from Argentina found that persistent loss of the sense of smell may be a better predictor of long-term cognitive and functional impairment than severity of the initial COVID-19 disease. In a large study population from nine Latin American countries, experiencing a positive life change during the pandemic, such as more quality time with friends and family, reduced the negative impact of the pandemic on memory and thinking skills. Finally, hospitalization in the intensive care unit (ICU) was associated with double the risk of dementia in older adults, according to Rush Alzheimer’s Disease Center in Chicago. These findings could be significant given the tremendous upsurge in ICU hospitalizations during the COVID-19 pandemic.
Ultra-Processed Foods May Speed Cognitive Decline
A study presented at AAIC 2022 finds that people who eat large amounts of ultra-processed foods have a faster decline in cognition. Researchers studied 10,775 people over eight years and found that high consumption (more than 20% of daily intake) of ultra-processed foods led to a 28% faster decline in global cognitive scores, including memory, verbal fluency and executive function. Ultra-processed foods go through significant industrial processes and contain large quantities of fats, sugar, salt, artificial flavors/colors, stabilizers and/or preservatives. Examples include sodas, breakfast cereals, white bread, potato chips and frozen “junk” foods.
Lower Socioeconomic Status, Persistent Low Wages Linked to Dementia Risk and Faster Memory Decline
Socioeconomic status (SES) — reflecting both social and economic measures of a person’s work experience, and of an individual’s or family’s economic access to resources and social position — has been linked to both physical and psychological health and well-being. Socioeconomic deprivation, including neighborhood disadvantages and persistent low wages, are associated with higher dementia risk, lower cognitive performance and faster memory decline, according to several studies:
- Individuals who experience high socioeconomic deprivation — measured using income/wealth, unemployment rates, car/home ownership and household overcrowding — are significantly more likely to develop dementia compared to individuals of better socioeconomic status, even at high genetic risk.
- Lower-quality neighborhood resources and difficulty paying for basic needs were associated with lower scores on cognitive tests among Black and Latino individuals.
- Compared with workers earning higher wages, sustained low-wage earners experienced significantly faster memory decline in older age.
- Higher parental SES was associated with increased resilience to the negative effects of Alzheimer’s marker ptau-181, better baseline executive function and slower cognitive decline in older age.
About the Alzheimer’s Association International Conference® (AAIC®)
The Alzheimer’s Association International Conference (AAIC) is the world’s largest gathering of researchers from around the world focused on Alzheimer’s and other dementias. As a part of the Association’s research program, AAIC serves as a catalyst for generating new knowledge about dementia and fostering a vital, collegial research community.
AAIC 2022 home page: www.alz.org/aaic/
AAIC 2022 newsroom: www.alz.org/aaic/pressroom.asp
AAIC 2022 hashtag: #AAIC22
About the Alzheimer’s Association®
The Alzheimer’s Association is a worldwide voluntary health organization dedicated to Alzheimer’s care, support and research. Our mission is to lead the way to end Alzheimer’s and all other dementia — by accelerating global research, driving risk reduction and early detection, and maximizing quality care and support. Our vision is a world without Alzheimer’s and all other dementia®. Visit alz.org or call 800.272.3900.
SOURCE Alzheimer’s Association
Learn more about Cadbury Commons’ Memory Care Program >
















You must be logged in to post a comment.